The reasons why Santé Kildare will not become a “Superclinic” any time soon


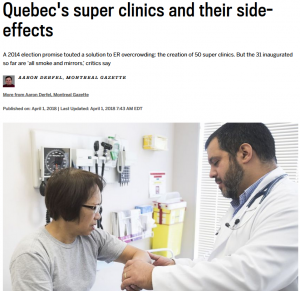
The Montreal Gazette recently published an exposé on “Quebec’s super clinics and their side-effects.” It’s hard to escape the hype with near weekly announcements by the Minister of Health touting these “new” establishments as a solution to ER overcrowding. Proponents call them the long-overdue solution to a chronic problem. Opponents call them “all smoke and mirrors.” I prefer the term “McMedicine” – Be wary of the adverse complications of Supersizing.
1. Superclinic ≠ Supercare
What’s in a name? Superclinics sounds spectacular – nurses with capes, doctors with superpowers. The Avengers the Primary Care!
However, we have to question who provides the care. This does not mean that superclinics don’t have super-doctors or super-nurses, but excellent care really emanates from a nurtured doctor-patient relationship. “Supercare” is delivered by the health team that knows you.
As Dr. Premji laments in healthydebate.ca – “We promote convenience over continuity.” In fact, “relational continuity” is associated with better care outcomes than speed.
2. We perpetuate myths about ER use
No doubt our ERs operate above capacity, but do superclinics solve the problem? As the Gazette correctly points out, ERs continue to work beyond recommended limits even with the weekly openings of new superclinics.
As Dr. Premji explains, we have to address and solve the underlying problems for ER overcrowding – such as overflowing inpatient wards, too few long-term care beds and an inadequate supply of home care services.
3. “All smoke and mirrors”
Superclinics did not apparate out of thin air. They are an extension of the pre-existing Clinique Reseau (CR) model established by Minister of Health Couillard more than a decade ago. Like superclinics, CRs were open on weekends and evenings with on-site access to radiology, labs and specialists. The difference – 4 hours on Saturday and Sunday.
Again the Gazette exposes the less-than-impressive truth: new superclinics may offer at least 40,000 consultations for walk-in patients each year (using the Pierre Boucher superclinic as an example), but the previously named Pierre Boucher Family Medicine Group had already surpassed that goal in 2016, reporting 47,000 consultations for walk-in patients that year!
4. It’s the PREMs!
If the acronyms CLSC, CSSS, CIUSSS, GMF, GMF-R, UMF are not confusing enough – consider the punitive PREMs. The Plans régionaux d’effectifs médicaux or PREMs, is a system the Ministry created to determine how many family doctors can practise in a specific area.
Sometimes access has nothing to do with hours – but with hiring adequate staff to meet the need.
As Dr. Mark Roper, Director of the superclinic at the Queen Elizabeth Health Complex comments: “We have doctors applying to work with us, but they are not permitted to work with us because of the government restrictions.”
The Gazette writes: “The PREMs, Roper argues, have tended to favor the outlying regions to the detriment of Montreal. Montreal doctors treat both local residents and those from the off-island suburbs who commute to the city, yet both Liberal and PQ governments have resisted allocating more permits to what is known bureaucratically as Region 6. Politically, more votes are up for grabs off island than in Montreal.”
5. Who is your clientele?
A big source of confusion remains who is responsible for care. Family Medicine Groups (GMFs) meet the needs of its defined, rostered population. Superclinics offer appointments to anyone. In an ideal world, superclinics bridge the gap between GMFs and ERs, but in reality, the system is contradictory, unnecessarily complex, and at times, adversarial.
Family doctors are financially penalized when their patients seek care elsewhere yet an aggressive advertising campaign for superclinics literally entice and lure patients away from their family doctors.
Combined with the fact that superclinics are also GMFs, the primary care equation becomes unrecognizable. Solve this formula: GMFs need 80% of its registered patients to see GMF doctors exclusively AND the same GMF-R (aka superclinic) is mandated to book non-registered patients 80% of the time! Care seems more paradoxical than complimentary.
6. Shuffling the deck
With PREMs limiting physician movement, who staffs the new wunderclinics? You guessed it – the same doctors from the GMFs, former CRs and even the ERs. As one family doctor commented to the Gazette – “I’m thinking of going to work in a super clinic, but that’s just a reshuffling of the cards, isn’t it?”
Other clinics (often the former CRs) are caught in GMF/GMF-R purgatory – too big for one yet small enough for the other. Funding is threatened and operators fear the demise of their services. One doctor notes, “It makes no sense. Since we want to create these super clinics, we’re in the process of hollowing out clinics that used to function well, clinics like mine.”
In the end, GMF Santé Kildare remains committed to providing supercare to our super-patients. We are fortunate to have a super-team committed to your health and wellbeing.